55 F with right sided weakness and slurring of speech
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
CASE PRESENTATION:
History taken by Dr. Aditya samitinjay
History is taken from the attenders as the patient is unable to speak.
A 60 year old lady presented with a 2 day history of progressive right sided weakness. The patient was feeling well until last Saturday afternoon when she complained of difficulty in mixing food which gradually progressed to an inability to clench her fist by that night. The next morning too this difficulty persisted and she reported that she was feeling dizzy and then suddenly lost her speech. At the same time, her daughter in law (our informant) reported that she noticed the patient was looking to one side and developed deviation of angle of mouth towards the right. The patient and the attendant then both noticed that she was completely unable to move her right sided limbs and she needed help in getting up from bed. The informant denied any history of bowel and bladder incontinence at that point, no history of irrelevant speech, no history of clutching of non existent objects in air, no history of sudden vision loss. Taken aback by the situation, the attendant immediately called her husband (patient's son) who rushed home. Understanding that the patient developed a 'stroke' they immediately brought the patient to our hospital in the afternoon.
A thorough review of past events was not significant for any history of memory loss prior to this, no history of antisocial behavior. No history of colliding with walls when walking. The informants deny a history of stuttering speech or loss of consciousness at any point in the course of events. They denied a history of severe headache, vomiting or fevers. They also denied a history of involuntary movements of limbs. They reported that the patient had a 4 month history of tingling with pins and needles sensation in her feet. Prior to this event, the patient denied a history of abnormal bowel or bladder habits, however they report that she woke up about 2 to 3 times in the night for passing urine, since about 4 to 5 months. Patient's son also told that she used to have disturbed sleep and used to wake up many times, on insisting why, he told that she used to say that she is getting nightmares. No history of stiffness of limbs. They report that the limbs are flaccid and she is even unable to stand with support, with buckling of her right knee. The informants do not recall any history of painful or painless sudden vision loss experienced by the patient. They however, report that she had been having progressively blurry vision which is painless. No history of scotoma was ever reported to them, no history of colored halos or loss of color vision. On review of systems, she had no history of vomiting or diarrhea, no history of pain abdomen. The informants recall a one year history of progression breathlessness with palpitations, which she described as a heavy feeling in her chest. They cannot recall PND or Orthopnea or chest pain before. The daughter in law reported that 5 months prior to this event, the patient had a reddish and intensely pruritic ulcer on her right foot. It was associated with mild pus discharge and initially of small size which gradually progressed to a larger sized lesion. They consulted a physician at that time and the lesion was debrided and the informants say that it eventually healed with scarring. The informants now report that both her feet appear discolored with a dark brown color. They don't recall the patient telling them of pain in the calves while walking or pain in her lower limbs at any point. The DIL also reported that her pedal edema back then was more on the right side but it was bilateral since 4 to 5 months. They deny a history of immobilisation or involuntary loss of weight or appetite. No past history of any surgical procedures in the last 1 year. The DIL recalls the edema was pitting type and on asking if she ever had morning facial puffiness, she confessed that the patient occasionally had a history of facial puffiness. On further questioningly, the DIL told us that she had a history of her footwear slipping and a feeling of numbness on the plantar surface of both her feet. She however never had a history of difficulty in walking in the dark. The DIL however, recalls the patient slipping on a really wet surface when taking the stairs and injuring her hip, which she says was uneventful.
The son reported that the patient had a 2 month history of cough with expectoration, it was bloody once, streaked on the yellow sputum. This was 4 months ago. He said that they consulted a physician who prescribed a cough syrup which brought no resolution. Another consultation about a week later at a government hospital was sought and at that point she was prescribed a one week course of antibiotics and symptomatic treatment with sputum sample taken for labs. The son regretfully informs that they did not bother following up with the physician at the hospital.
The patient is an elderly lady with 2 children, the informant is her eldest child (son) and she also has a daughter whom she got married 5 years ago. She has stopped working for the past 2 to 3 years largely because she was feeling fatigued than before. The son denies a history of fevers, night sweats or any unusual swellings or masses on her body. She hasn't received a formal education and her finances are managed by her son, who took over when his father died of an alcohol problem 8 years ago. She previously had a fairly balanced diet with a good mix of vegetarian and non vegetarian food.
H/o cataract 5 years back for which she was operated but son says it was unsuccessful.
No pallor, icterus, cyanosis,clubbing,lymphadenopathy,
B/L pedal edema is seen.
Vitals:
Bp=190/90 mm Hg
PR=130 bpm, irregularly irregular
RR=38 cpm
Spo2=97%
GRBS=437 mg%
Systemic examination:
CVS:
Apex beat cannot be visualized
Visible jugular and carotid pulsations on right side
Irregularly irregular pulse
S1, S2 heard, No murmurs, irregular heart beat
CNS:
Speech:Unable to speak
MMSE:cannot be assessed as she has difficulty in speaking
Cranial nerve examination:
1st cranial nerve --cannot be examined
2nd cranial nerve- direct and indirect light reflexes are present
3rd, 4th, 6th:
Pupil size- RT LT
N N
No Nystagmus, ptosis
5th:
Sensory -cannot be examined
Motor(corneal,conjunctival) +ve +ve
7th:
Sensory-cannot be examined
Deviation of mouth towards left side
8th:
Rinne's test ,Weber's test-cannot be examined
9th, 10th:
Palate: cleft palate
11th:
Trapezius, SCM not elicited
12th:
Tongue-not elicited
Superficial reflexes:
Rt Lt
Corneal p p
Conjunctival p p
Abdominal - -
Plantar Dorsiflexion plantarflexion
Deep tendon reflexes :
Biceps p p
Triceps A A
Supinator A A
Knee A p
Ankle A A
Sensory system:Not elicited
Pain present in both right and left upper and lower limbs.
Cerebellum:
Finger nose test-Negative
Nystagmus -Absent
Tone:
Hypotonia in right UL and LL
Power:
UL RT LT
Shoulder 0/5 3+/5
Elbow 0/5 4-/5
wrist 0/5 3+/5
Hand grip 0/5 85-90%
LL
Hip 0/5 3+/5
Knee 0/5 3+/5
Ankle 0/5 3+/5
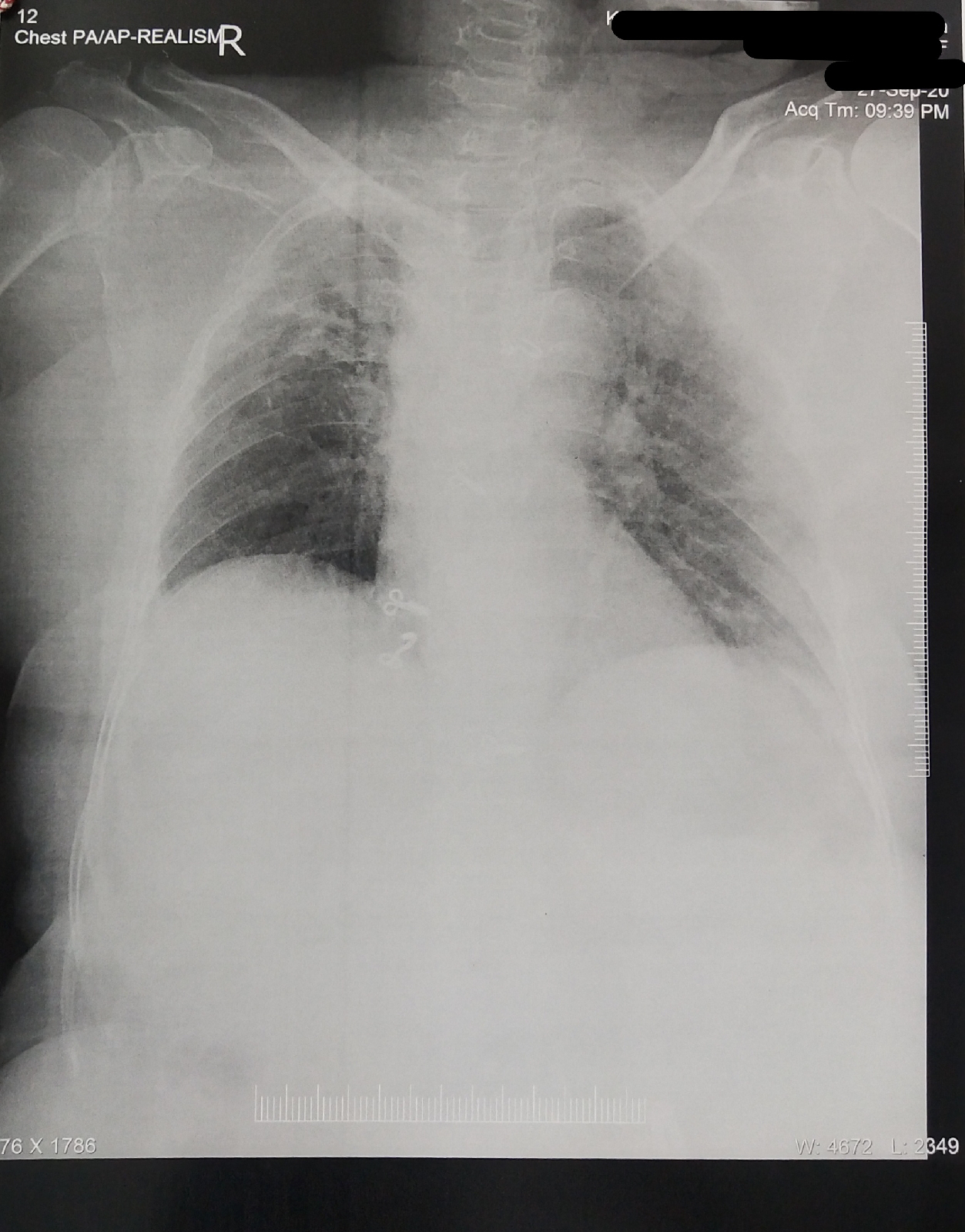
RS: BAE + crepitations are heard in right and left infra clavicular,right and left infra scapular regions
P/A:
Soft, Non tender, No organomegaly Bowel sounds heard
27/9/2020:
Investigations:
Rx:
Tab.Ecospirin 300 mg stat
Tab. Atorvas 40 mg PO/HS
BP -2nd hrly monitoring
GRBS, Spo2 monitoring-4th hrly
I/O charting
28/9/2020
2D Echo report:
Ef=50%
Good to fair LV function
No RMWA, no MS/AS
Mild TR
No MR/AR
Diastolic dysfunction+
Patient may have right sidedcomplete hemiplegia with cardioembolic stroke due to MAT secondary to Rt ULL Fibrosis (?TB). De novo detected DM Type 2 and HTN with Diabetic Triopathy and Diabetic Dermopathy.
O/E:
Patient is conscious, coherent, cooperative
Afebrile
Bp:140/80 mm Hg taken in supine position of right arm
PR:65 bpm, irregularly irregular
Spo2:98% at RA
GRBS:199 mg/dl
No pallor,cyanosis
Cvs:S1,S2 +
RS:BAE + , clear
Rx:
Tab. Ecospirin 75 mg PO/OD
Tab. Atorvas 20 mg PO
BP, Spo2 monitoring 4th hourly
I/O charting
Physiotherapy of right upper limb and lower limb
Inj. HAI
Inj. Amiodarone 150 mg IV stat
Inj.KCL 1 ampoule in 100 ml NS over 6 hrs
Syp. Lactulose 15ml PO/OD
Tab. Met xl 25 mg PO/OD
29/9/2020
O/E: patient is afebrile
Bp:140/80 mm Hg taken in left arm in sitting position
PR:84 bpm irregularly irregular
Cvs :S1, S2 heard
Rx:
Tab.Ecospirin 75 mg PO/OD
Tab. Atorvas 20 mg PO/HS
Inj. HAI SC
Syp. Lactulose 15 ml OD/PO/HS
Tab. Met xl 25 mg O
30/9/2020:
Bp-160/80 mm Hg taken in sitting position in right arm
PR-61 bpm, irregularly irregular
RR-25 cpm
Investigations:
Rx:
Tab. Ecospirin 150 mg/PO/OD
Tab. Atorvas 20 MG PO/HS
INJ. HAI S/C
SYP. Lactulose 15 ml/PO/OD/HS
Tab. Met XL 25 mg/PO/OD at 8 am
GRBS monitoring
Inj. Ceftriaxone 1 gm/IV/BD
Physiotherapy of both UL and LL
1/10/202
Patient is afebrile
BP:140/90 mm Hg taken in right arm in supine position
PR: 92 bpm
Spo2: 98%
GRBS: 184 mg% (8 am)
CVS :S1, S2 heard, no murmurs
RS: BAE + crepts heard in right infraclavicular and B/L infra scapular areas
Rx:
Tab. Ecospirin 150 mg OD
Tab. Clopidogrel 75 mg OD
Tab.Atorvas 20 mg H/S
Inj. HAI s/c
Syp. Lactulose 15 ml H/S
Tab. Met XL 25 mg OD
Inj. Ceftriaxone 1gm BD
Tab. Metformin 500 mg OD
physiotherapy