45 M with shortness of breath since two years
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
Case presentation:
History is taken from patient's wife as patient is not able to talk.
A 45 year old male, auto driver by occupation complaints of sudden onset of shortness of breath post dialysis(2/10/2020) since 3 am on 3/10/2020.
Patient was apparently asymptomatic 3 years back when one day around 6pm he met with road traffic accident and had fracture of right lower limb. For the fracture rod (Nailing and plating) was inserted.He was incidentally found to have subclinical hypothyroidism with TSH being high than normal range and T3, T4 being normal and creatinine being 1.9 and then he was on Tab. thyronorm 25 mg for about 2 months and stopped it as he was subjectively feeling better.After which for about a year he took rest and later for 6 months he worked as a tractor driver without any complaints with total normal lifestyle. Then 1 and half year back he went to a local hospital near their residence with complaints of shortness of breath(grade 3),cough,palpitations. Patient's wife gives history that he used to wake up from his sleep and sits and after a few minutes it used to subside. And after a few days his shortness of breath is aggravated on lying down and decreases while in sitting position.It was dry cough & No aggravating and relieving factors. There the patient underwent few tests and found ser.creatinine being 3.25 and also was diagnosed with dilated cardiac myopathy with reduced ejection fraction from 60% to 40% and he was given medication (unknown). And at the same time patient was diagnosed with hypertension (he was on tab. Amlong 10) They were also told that patient has kidney infection and can become better with medication (unknown).There after he stopped driving tractor and bought an auto and worked as driver for 1 year. Patient was on regular medication but 8 months back because of financial crisis and he stopped taking medication for 2 months. And after 1 month he started losing his appetite and also associated with loss of around 10 kg of weight.patient has no history of night sweats . After that when he was again attacked with shortness of breath,one and half month back they came to Kamineni hospital where the patient was told his kidneys are malfunctioning and asked to get dialysis through AV fistula. For this reason they went to Hyderabad. After 5 days he again came to Kamineni hospital for further evaluation. Patient was diagnosed with asthma 1 year back (uses inhaler whenever necessary).
He had his first dialysis on 9/9/2020. And had his last dialysis on 3/10/2020.
Patient had three sessions of dialysis thereafter on 6/10/2020, 9/10/2020,12/10/2020
Not a k/c/o diabetes, tuberculosis,seizures, CVA, CAD.
Patient was on mixed diet, eats only twice daily once in the morning around 10 am and then at night around 8 pm. He goes to work after having his breakfast and returns home by 7:30 pm. Patient usually sleeps around 10 for a minimum of 5-6 hours. Patient started consuming alcohol since 25 years of age. He consumes about 90 ml of alcohol daily. Not a smoker. He was married twice. He married his late wife 20 years back and had two sons with her. Later she was diagnosed with leukemia and died because of it. Later he married his current wife (informant) 8 years ago. He had a son with her. Patient has no sleep disturbances and his bowel movements were regular.
In view of falling saturation patient was intubated.
At around 8:30 am in view of falling heart rate CPR was started immediately according to 2015 AHA guidelines.Inj.Adrenaline 1 mg IV stat given. BP and PR normal. Another dose of Inj. adrenaline given after 5 min. Pulse rate recordable and ROSC established. Pink sputum is present.
O/E:
Patient is under conscious
Vitals:
BP-150/90 mm Hg taken in supine position in right arm
PR-107 bpm
Spo2-100% on ventilation
CVS: S1, S2 heard, no murmurs
Jugular venous pulsations are visible
RS: BAE +, fine creptiations are heard in B/L infra clavicular and B/L infrascapular areas.P/A:soft, non tender, no organomegaly, bowel sounds +
Patient may have CKD with MHD with pulmonary edema secondary to hypertensive urgency and ROSC with T1 respiratory failure
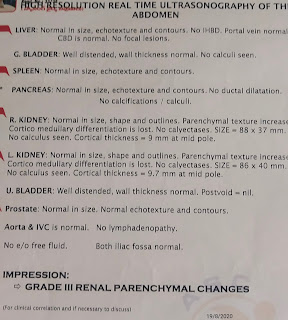
Investigations:
3/10/2020